Karen Ann Quinlan Hospice welcomed and gave thanks to all the Veterans that joined us at the “Welcome Home Vietnam Veterans Day” luncheon and ceremony. All Veterans, including all branches and service periods, are always welcomed at this event. The Vietnam War Veterans Recognition Act designates March 29 of each year as National Vietnam War Veterans Day, although states celebrate “Welcome Home Vietnam Veterans Day” on March 29 or 30 of each year.
Author Archive: Stace Schimpf
Hospice Care, What Is It?
Posted on by Stace Schimpf
What is Hospice?
Hospice helps patients and families focus on living. Hospice care brings comfort, dignity, and peace to help people with a life-limiting illness live every moment of life to the fullest. It also reaches out to provide support for the family and friends who love and care for them.
Hospice provides expert medical care, pain management, and emotional and spiritual support. With Hospice comes an entire team that works together focusing on the patient’s needs whether physical, emotional, or spiritual. Support is provided to the patient’s loved ones as well.
The goal is to keep the patient as pain-free as possible, with the loved ones nearby. Addressing pain and other symptoms in their early stages, rather than waiting until they become severe, is a priority. In addition to determining the appropriate medications for pain and other symptoms, members of the care team identify the best ways to administer the medication to the satisfaction of the individual patient.
When is the right time for Hospice?
A growing number of caregivers are finding that the correct answer to the question is, “As early as possible,” as they discover all of the advantages hospice has to offer the patient as well as the caregivers. Hospice professionals are specialists in end-of-life care, and should be called upon during the first stages of a terminal illness.
Our hospice staff is trained to offer peace of mind in addition to medical care. We hear it so many times, patients and families tell us: “We wish we’d called hospice sooner.” Patients and families can benefit most from hospice care when they seek support earlier rather than in a crisis.
Special needs require the services of specialists. Hospice professionals are specialists in end-of-life care, and should be called upon during the first stages of a terminal illness.
Who is on the Hospice Care Team?
A Hospice team usually consists of:
- Chaplains or other counselors
- Certified Home Health Aides
- Hospice Physicians
- Nurses
- Social Workers
- Volunteers
- Bereavement Counselors
Often times, patients choose to have their primary doctor involved in hospice care. Both the primary doctor and the hospice medical director may work together to coordinate the patient’s medical care, especially when symptoms are difficult to manage.
In most cases, Hospice care is provided in the patient’s private residence, but may also be provided in freestanding hospice facilities, hospitals, nursing homes, assisted living facilities, or other long-term care facilities.
Although hospice provides a lot of support, the day-to-day care of a person receiving hospice care is usually provided by family, friends, or privately paid home health aides. The hospice team coaches caregivers on how to care for the patient and even provides respite care when caregivers need a break.
While family members are usually the primary caregivers for hospice patients, members of the hospice staff make regular visits to assess the patient and provide additional care or other services and hospice staff are on-call 24 hours a day, seven days a week.
What services come with Hospice care?
Hospice offers social workers and counselors to help the family make emotional adjustments to the illness and its progression. They also can offer guidance in living wills and advance directives. Chaplains offer spiritual support as requested. Certified home health aides help by providing patient physical care and hygiene. Trained volunteers offer assistance and companionship for the patient and the family. Therapists, dieticians, special equipment needs and pharmacists are also available.
Other important benefits that come with hospice to keep in mind:
- Management of pain and other symptoms
- Assistance for patients and loved ones with the emotional, psychosocial, and spiritual aspects of dying
- Medications and medical equipment
- Instructing the family caregivers on how to care for the patient
- Grief support and counseling to the patient as well as the surviving family and friends for up to 13 months after death
- Hospice meets patients where they are, whether that is in a skilled nursing home, assisted living facility, hospital, the home of a loved one or in their own home.
- Hospice patients and families can receive care for six months or longer.
- To get the most out of what hospice offers, it’s better to have care for more than just a few days.
The best time to learn about hospice is BEFORE you or your loved one needs it.
Six Months or Longer
Posted on by Stace Schimpf

Former President Jimmy Carter died recently at the age of 100 after being on Hospice care for nearly two years.
How can that be? According to Medicare guidelines, to qualify for hospice under Medicare a patient must have a prognosis of six months or less to live if the disease runs its normal course. What if a patient lives longer then six months… won’t they lose hospice care?
Not necessarily.
Hospice patients and families can receive care for six months OR LONGER. In August 2023, President Carter reached the six-month milestone on hospice and continued to enjoy time with his family and loved ones in his hometown of Plains, Georgia.
Some patients outlive their prognosis, and in those cases the patient can be recertified for continued hospice care. You can get hospice care for two 90-day benefit periods, followed by an unlimited number of 60-day benefit periods.
Studies have shown that hospice patients tend to live longer than patients with similar diagnoses who do not choose hospice care. Research also shows that hospice care—at any length of stay—benefits patients, family members, and caregivers, including increased satisfaction and quality of life, improved pain control, reduced physical and emotional distress, and reduced prolonged grief and other emotional distress.
Hospice care focuses on quality of life when a cure is no longer possible, or the burdens of treatment outweigh the benefits. Some people think that their doctor’s suggestion to consider hospice means that death is very near. That is not always the case. In fact, people often don’t begin hospice care soon enough to take full advantage of the help it offers.
Talk with your doctor if you think a hospice program might be helpful for you or a loved one.
One last thing to keep in mind, it is possible to leave hospice care if a patient’s condition improves or they decide they wish to resume curative care and return to hospice care later.
Make Your Wishes Known
Posted on by Stace Schimpf

The NHPCO helps decode Advanced Care planning documents
Over time, several types of documents have emerged to help you express your wishes for treatment any time you are unable to speak for yourself, particularly during serious illness or end of life.
Certain words, like “Living Will” and “Advance Directive”, are used interchangeably when they should not be.
Others, like “Healthcare Power of Attorney”, have about five different names.
None require the advice or services of an attorney to create. Some are legal documents, some are medical orders some are valid outside of the hospital and some are not. Some everyone should have and others are applicable only towards the end of life. All, however, are only useful if they are accessible when you need them and if the person you have authorized to speak for you is empowered to do so. Let us help you sort it out.
What are Advance Directives?
Advance Directives are a set of documents that both appoint a person to speak for you and contain your preferences for medical treatment. Each state has its own Advance Directive with the language and content that state deems important.
All Advance Directives must include at least two sections:
- A statement of your preferences for medical treatment (or not), also known as a Living Will and
- The appointment of a person to speak for you if you are unable to, also known as a Healthcare Agent.
In other words, a Living Will is one component of an Advance Directive.
Advance Directives may also contain instructions around organ donation, appointment of a guardian, and other matters.
Are Living Wills the same as Advance Directives?
A Living Will is a statement of the type of care you prefer if you are not able to speak for yourself. It is important to understand that living wills only apply to your healthcare wishes; you will need something called “a last will and testament” to express your wishes about what to do with material goods.
While each state has state-specific Advance Directive form, there aren’t separate state-specific Living Will documents because the information contained in a Living Will is already part of the Advance Directive. Nonetheless, just to make things even more confusing, a lot of the websites that offer “‘free”’ legal forms online incorrectly refer to Advance Directives as Living Wills. A Living Will, without having appointed someone to speak for you, is of limited value. Frequently, the decisions that need to be made are not specifically addressed in the Living Will. Your Healthcare Agent is in the best position to know what you would want and is authorized to speak for you.
What are Healthcare Powers of Attorney?
A Healthcare Power of Attorney can be both a person and a legal document. The legal document appoints and authorizes someone to speak for you when you cannot and must be witnessed or notarized, depending on where you live. The person, the Healthcare Power of Attorney, may also be known as a Healthcare Agent, Healthcare Proxy, Healthcare Surrogate, Healthcare Attorney in Fact, or Healthcare Representative. Each state has its own Healthcare Power of Attorney form, which is embedded in that state’s Advance Directive.
What are DNRs?
Do Not Resuscitate orders (DNRs) are medical orders written by a doctor. They instruct healthcare providers not to do cardiopulmonary resuscitation (CPR) if a patient’s breathing stops or if the patient’s heart stops beating. If presented, they will be honored by EMTs.
They may be part of a POLST but can also be their own form.
What are POLSTs?
POLST is an abbreviation for Physician’s Orders for Life-Sustaining Treatment. POLSTs are forms that consist of a set of medical orders that applies to a limited population of patients, such as seriously-ill or frail persons, and address a limited number of critical medical decisions.
A POLST has the option of specifying Do Not Resuscitate (DNR) but also makes provisions for other types of treatment such as feeding tubes and mechanical ventilation. They will be filled out in consultation with your doctor. POLSTs are state-specific and are specifically for the seriously ill or frail. If presented, they will be honored by EMTs.
POLSTs do not appoint someone to speak on your behalf like Advance Directives do.
Your Healthcare Agent is the person that can speak for you when you cannot; they are your legal representative and the doctors must listen to them. However, it is also useful to fill out a HIPAA Right of Access to Healthcare Information for anyone you want involved in your care.
What is a HIPAA Right of Access to Healthcare Information?
The Health Insurance Portability and Accountability Act of 1996 (HIPAA) is a federal law that required the creation of national standards to protect sensitive patient health information from being disclosed without the patient’s consent or knowledge. Keep in mind, if you have several people that you would like to be empowered to speak with your doctors they will each need an authorization.
What do I need to decide?
There are three decisions to make and actions to take that will help you get what you want (and not get what you don’t want) when you are unable to speak for yourself. The decisions, and their respective tasks, fall into:
- Deciding on and appointing someone to speak for you when you can’t
- Getting clarity about what you want and don’t want. This includes giving specific instructions around resuscitation, ventilation, and feeding if appropriate for your stage of life.
- Telling your agent and others what you want, writing it down, and having the information available when needed
National Hospice and Palliative Care Month
Posted on by Stace Schimpf

November is National Hospice and Palliative Care Month. Announced in 1978 by then President Jimmy Carter, November is a time to raise awareness about the importance of hospice and palliative care services, and to honor the caregivers and healthcare professionals who provide them. While HAPCM is a brief window of time meant to spotlight the importance of hospice and palliative care, helping the public understand the benefit of this type of serious-illness care and the importance of advance care planning are goals which our community should strive for year-round.
Some key observances during the month include:
-National Family Caregiver’s Day: November 1
-Palliative and Advanced Care Week: November 4-8
-Hospice Week: November 11-15
-Home Health Week: November 18-22
-Private Duty Home Care Week: November 25-29
Hospice care enables the individual and their families to experience the final stage of life together, in the setting most comfortable for them. In most cases, the person remains at home, close to family and friends while under professional medical supervision, but hospice Research shows that families of hospice patients are more likely than non-hospice patients to report that their loved ones had their end-of-life wishes fulfilled.
What Type Of Support Can Hospice Care Offer?
Posted on by Stace Schimpf

Hospice provides support and comfort for people who need end-of-life care. Opting for hospice care is one of the most compassionate decisions you will ever make.
You can receive hospice care in your own home, a residential facility, such as the Karen Ann Quinlan Home for Hospice in Fredon, or in assisted living centers, nursing homes and hospitals. Some patients receive care in the homes of friends or family.
According to the Hospice Foundation of America, a third of all Americans choose hospice care when they are dying. But hospice isn’t only for the dying. Loved ones also benefit from hospice care, as the hospice team will support them through some of the most difficult moments in life.
Here are some of the support services you can expect from Karen Ann Quinlan Hospice:
• Every patient who receives hospice treatment must be qualified by a physician; all care is directed by your primary physician.
• Nursing care and services are provided by or under the supervision of a registered nurse. At Karen Ann Quinlan Hospice our nursing staff is available to patients and families 24-hours a day.
• Social Services are provided by a qualified social worker under the direction of a physician.
• Assists the patient and family members with the emotional, psychosocial, and spiritual aspects of dying
• Guides the family on how to care for the patient
• Offers short-term inpatient care when pain or symptoms become too difficult to manage at home, or the caregiver needs respite time
• Our hospice Medical Director will oversee the general needs of the patient working in tandem with the attending physician which includes palliation and management of the terminal disease and related conditions.
• Home Health Aides provide personal care services. Aides’ services are provided under the general supervision of a registered nurse.
• Chaplain Services are available to provide/facilitate spiritual counseling.
• Volunteer services are available to assist the patient/caregiver in any one of a multitude of ways from providing comfort and respite to the family, an avenue of socialization for the patient; assistance with shopping, etc. All volunteers have completed a Karen Ann Quinlan Hospice training course.
• Bereavement Services are provided for 13 months following the patient’s death to family and significant others. Additionally, the Joseph T. Quinlan Bereavement Center holds bereavement and grief recovery support groups in all the communities served by Karen Ann Quinlan Hospice.
• The staff at Karen Ann Quinlan Hospice is trained to offer peace of mind in addition to medical care.
We hear it so many times, patients and families tell us: “We wish we’d called hospice sooner.” Patients and families can benefit most from hospice care when they seek support earlier rather than in a crisis. The best way to determine if you or your loved one could be helped by hospice is to call us at 800-882-1117.
Wine and Cheese Festival Photo Gallery
Posted on by Stace Schimpf
What is a Death Doula?
Posted on by Stace Schimpf

In a recent story published by the NHPCO, they addressed the question, “What is a Death Doula?”
While hospice and palliative care provide physical end-of-life care for patients and their loved ones, a death doula — or end-of-life doula — can enhance traditional care by offering an additional layer of support. Death doulas provide non-medical emotional, spiritual, and physical support to individuals who are transitioning to death, and their loved ones.
As hospice and palliative care focus on pain and symptom management for patients and their loved ones, death doulas can often help those facing the end of life achieve a better death by allowing them to live the time they have left with purpose and companionship.
The word “doula” originates from a Greek word meaning “a woman of service,” and was later adopted by those guiding women through their birth process in a term used widely today: birth doula. The titles “death doula” or “end-of-life doula” are the most common terms for the type of practitioner described here, but you may also hear a death doula referred to as a death midwife or an end-of-life coach.
Central to the doula’s role is non-judgmental, holistic support that empowers patients and their loved ones to make the choices they want for their death experiences and to do so surrounded by the support they need. Doulas work to create and hold space for the needs and wishes of the dying while at the same time using their expertise to bring perspective, greater meaning, and comfort to the dying process.
Who can benefit from a death doula?
Anyone nearing the end of life can benefit from a death doula, and death doulas can begin working with patients and/or their families at any point in the death process. Some will choose to engage with an end-of-life doula as soon as they learn of a terminal diagnosis or receive a prognosis with limited time, though doulas are not bound to the six-month-or-less prognosis that hospices must abide by. Others will choose to integrate a death doula when they are closer to death, using their services for emotional and spiritual peace during a more difficult phase. Others still may engage a doula after the death of a loved one for support through the grieving process.
Doula services can be provided alone or in conjunction with traditional healthcare services—like hospice care and palliative care—to enhance the patient and family’s experience.
What services might a death doula offer?
The services that each doula offers depend on their skill set and training. Below are some of the core services an end-of-life doula may provide, though this list is not exhaustive. If you’re looking for a death doula that is right for you or your loved one, be sure to ask which services they furnish to ensure they can meet your unique needs.
• An explanation of common signs and symptoms of the dying process, as well as their meanings
• Help exploring the meaning of the dying person’s life and legacy
• An open ear to receive the frank thoughts of the dying, and provide counsel if requested
• Companionship during the death process – many doulas sit vigil so those in the death process are not alone
• Appropriate, comforting touch and massage
• Caregiver assistance and respite as well as emotional support
• Referrals for patients and family members to additional community resources or care providers, as needed
• Practical support through errands, household help, transportation, etc.
• Grief support for the bereaved
2024 Butterfly Release Photo Gallery
Posted on by Stace Schimpf
National Healthcare Decisions Day
Posted on by Stace Schimpf

Published by: National Hospice and Palliative Care Organization
National Healthcare Decisions Day, which is dedicated to inspire, educate and empower the public about the importance of advance care planning, is recognized each year on April 16. The goal is to engage everyone in conversations that encourage people to start to think about their own personal wishes for their health care, particularly at the end of life, and getting people to plan ahead, document those plans, and let loved ones know their wishes.
Advance care planning involves making future healthcare decisions that include more than deciding what care you would or would not want; it starts with expressing preferences, clarifying values, and selecting an agent to express healthcare decisions if you are unable to speak for yourself.
National Healthcare Decisions Day is a collaborative effort of national, state and community organizations committed to ensuring that all adults with decision-making capacity in the United States have the information and resources to communicate and document their future healthcare decisions.
In honor of National Healthcare Decisions Day, NHPCO encourages everyone to:
Have A Conversation
Advance care planning starts with talking with your loved ones, your healthcare providers, and even your friends- all are important steps to making your wishes known. These conversations will relieve loved ones and healthcare providers of the need to guess what you would want if you are ever facing a healthcare or medical crisis.
Complete Your Advance Directive
“Advance Directives” are legal documents (Living Will and Healthcare Power of Attorney) that allow you to plan and make your own end-of-life wishes known in the event that you are unable to communicate.
Engage Others in Advance Care Planning
Share brochures, information and advance directives to others in your family, workplace and community. Help others have a conversation about advance care planning.
“National Healthcare Decisions Day exists to inspire, educate and empower the public and providers about the importance of advance care planning.”
Remember….. Your Decisions Matter!
Taking time to listen as a Caregiver
Posted on by Stace Schimpf

The many tasks of caregiving can be so overwhelming that you just start doing things, maybe before you have really taken in what actually needs to be done. It is important to take the time to listen—to the person you are caring for, to the other people caring for them, and to yourself.
Listening to the Patient
You may be caring for someone who needs assistance with day-to-day chores and tasks but can still make their own decisions about personal matters such as medical care, financial and household issues. Take some time to listen and explore what kind of help they want. Often what we think someone wants or ought to want is not what they want at all. Sometimes people resist asking for help, even when it is clear they would benefit from assistance. If that is the case, start small and know that over time things will change as they learn to talk with their inner circle and realize what they want help with.
Knowing and understanding what someone wants will be important if you become responsible for making decisions for them. Read up on advance directives which will help you talk about medical decisions and fill out the documents. Not every situation can be anticipated so it is helpful to understand in general what is important to the patient—what they see as quality of life.
Listening to the doctors and other healthcare workers
You can offer to go to appointments with the patient and assist by taking notes and keeping track of papers, reports and prescriptions as you and the patient talk to the doctor. Take along the list of questions you generated together. Check with the patient during the appointment to be sure they are getting the information they want and need. Repeat back to the doctor any instructions to be sure they have been understood correctly.
Listen to yourself and reach out for information and support
Caregiving can be quite rewarding, and it can be quite challenging. Try not to have rigid expectations of how it will go or how you will feel. Showing up is good; perfection is the enemy. There are resources available to caregivers through government sponsored websites like MyHealthfinder as well as private organizations such as AARP and Caregiver Action Network.
Seek support groups of people caring for like patients; there are many online and in person. The National Institute of Aging, the CDC, the National Alliance on Caregiving, and AARP all are rich resources for help and connections. The American Cancer Society, the American Heart Association, and the Alzheimer’s Association as well as many other disease specific associations all have good information for caregivers.
Ten Things You May Not Know About Hospice Care.
Posted on by Stace Schimpf
 Some people mistakenly think hospice care is just about dying…that hospice is the place you call when there’s nothing more that can be done. Nothing could be further from the truth. Hospice helps patients and families focus on living. Hospice care brings comfort, dignity, and peace to help people with a life-limiting illness live every moment of life to the fullest. It also reaches out to provide support for the family and friends who love and care for them. According to the NHPCO, in 2021 1.71 million Medicare beneficiaries were enrolled in hospice care for one day or more.
Some people mistakenly think hospice care is just about dying…that hospice is the place you call when there’s nothing more that can be done. Nothing could be further from the truth. Hospice helps patients and families focus on living. Hospice care brings comfort, dignity, and peace to help people with a life-limiting illness live every moment of life to the fullest. It also reaches out to provide support for the family and friends who love and care for them. According to the NHPCO, in 2021 1.71 million Medicare beneficiaries were enrolled in hospice care for one day or more.
There are some important facts about hospice that people don’t know and this may be stopping people from getting the best care possible, when they need it most:
1. Hospice is not a place; it’s high-quality medical care that helps the patient and family caregivers focus on comfort and quality of life.
2. Hospice is paid for by Medicare, Medicaid, most insurance plans, HMOs, and managed care plans. Fear of costs should never prevent a person from accessing hospice care.
3. Hospice serves anyone with a life-limiting illness, regardless of age or type of illness.
4. Hospice serves people of all backgrounds and traditions; the core values of hospice—allowing the patient to be with family, including spiritual and emotional support, treating pain—cut across all cultures.
5. Research has shown that the majority of Americans would prefer to be at home at the end of life’s journey—hospice makes this possible for most people.
6. Hospice serves patients in hospitals, nursing homes, private facilities, or our Karen Ann Quinlan Home for Hospice; however most hospice care is given in the patient’s own home.
7. Hospice patients and families can receive care for six months or longer.
8. A person may keep his or her referring physician involved while receiving hospice care.
9. Hospice offers grief and bereavement services to family members and the community.
10. To get the most out of what hospice offers, it’s better to have care for more than just a few days.
If this information about hospice surprises you, take the time to find out more. The best time to learn about hospice is BEFORE someone in your family is facing a healthcare crisis. For more information, contact Karen Ann Quinlan Hospice at 800-882-1117. This information is provided by the National Hospice and Palliative Care Organization and Karen Ann Quinlan Hospice. Karen Ann Quinlan Memorial Foundation is passionately dedicated to providing Hospice care for the terminally ill and Bereavement for those who have lost loved ones.
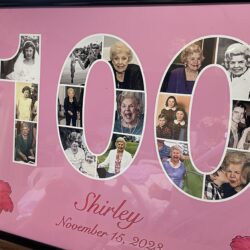
Happy Birthday Shirley!
Posted on by Stace Schimpf
This week Karen Ann Quinlan Hospice had the honor of sharing in the 100th Birthday of Shirley B. Her family celebrated with a banner, old photos, custom chocolate treats, flowers and balloons to help mark her special day. Grandchildren and other family members who couldn’t be with her for the celebration called her on the phone and some even reached out to her over video chat to extend their love and well wishes!
Shirley was born in 1923 in Amber, NY, and grew up in Skaneateles, NY. Shirley met her husband while at nursing school in Syracuse, NY. They were married in 1946 and had 4 children. As newlyweds, they lived in Syracuse, but eventually moved to Sparta, NJ, where they lived for about 50 years. At her birthday celebration Shirley spoke very fondly of Sparta; she loved living there!
Over the years, her family grew to 9 grandchildren and 5 great-grandchildren.
A dedicated healthcare professional, she worked as a Registered Nurse in Andover, NJ, and Newton, NJ, until the age of 89 years old.
Shirley spent the last 50 years as a member of the Lafayette Federated Church. For many years, countless people gathered in her home for Prayer Group and she also met with friends for weekly prayer. Her philosophy was that every day was a gift and her prayer was always that God would use her to be a blessing to all she would encounter throughout her day, as a nurse, mother, friend or stranger.
Happy 100th Birthday Shirley!
November is National Hospice and Palliative Care Month
Posted on by Stace Schimpf
The NHPCO recognizes National Hospice and Palliative Care Month
November is recognized annually as National Hospice and Palliative Care Month (HAPCM), a time for providers to reach out to their local communities, engage media contacts, and recognize the valuable contributions made by staff and volunteers. While HAPCM is a brief window of time meant to spotlight the importance of hospice and palliative care, helping the public understand the benefit of this type of serious-illness care and the importance of advance care planning are goals which our community should strive for year-round.
Each year, the National Hospice and Palliative Care Organization (NHPCO), establishes a theme for the month and creates outreach materials for members. The theme for HAPCM 2023 is Courageous Conversations.
In a culture that often teaches us to resist mortality and a healthcare system defined by , the seemingly simple act of having a conversation about dying can have a profound impact. What does death mean in my life? If I am faced with a terminal diagnosis, how would my values shape my end-of-life journey? How do I want my loved ones to engage with me toward the end of my life? It’s difficult to think about these questions but having these courageous conversations with ourselves, family, friends, and doctors can mean the difference between having the type of death a patient wants – one that matches up with their values and desires – and one that doesn’t allow them to have a say in their own end-of-life journey.
Throughout the month, NHPCO is encouraging everyone to have these Courageous Conversations to start a meaningful dialogue on “dying a good death.”